Table of Contents
What is Psoriasis?
Psoriasis is a long-lasting autoimmune disease characterized by patches of abnormal skin. These skin patches are typically red, itchy, and scaly. They may vary in severity from small and localized to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as the Koebner phenomenon. Psoriasis is associated with an increased risk of psoriatic arthritis, lymphomas, cardiovascular disease, Crohn’s disease and depression.
What are causes and risk factors of Psoriasis?
The cause of psoriasis is not fully understood; however, it is believed to have a genetic component and there are many environmental factors that may trigger a flare. Individuals who carry certain human leukocyte antigen (HLA) alleles are more likely to develop psoriasis than those who do not. Psoriasis has been linked to cardiovascular disease and other comorbidities. The risk of developing these diseases appear to be higher in people with severe psoriasis compared to patients with mild psoriasis.
The exact cause of psoriasis is unknown. It is believed to be caused by a combination of genetic and environmental factors. The risk factors include:
- Family history (genetics)
- Stress
- Smoking tobacco
- Heavy alcohol consumption
- Infection
- Obesity
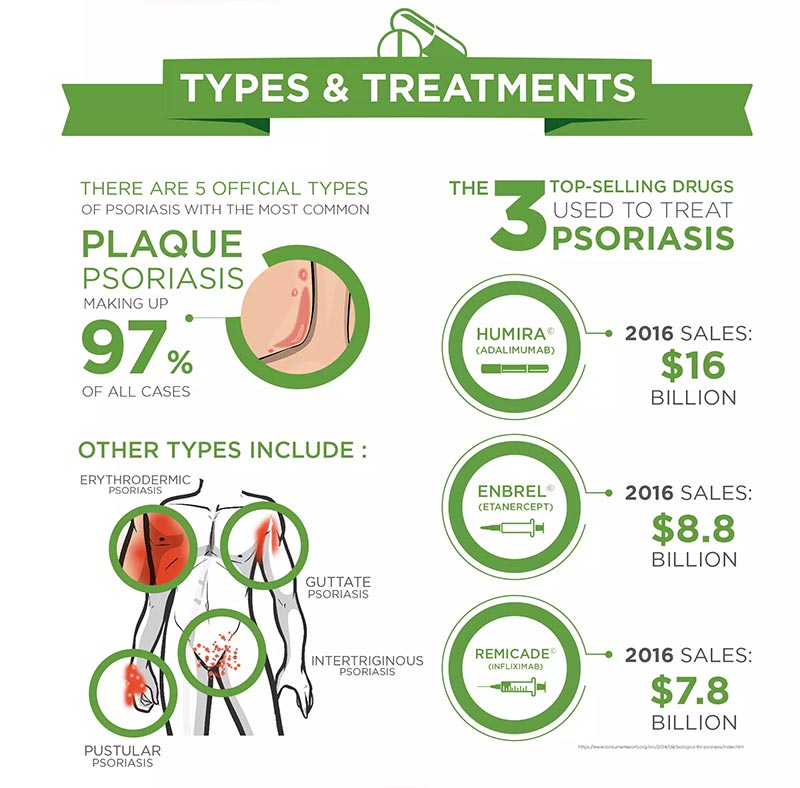
What are the different types of Psoriasis?
Plaque psoriasis (psoriasis vulgaris) is the most common form of psoriasis. It involves red patches of skin with white scales. The patches often appear on the scalp, knees, elbows and lower back, but they can show up anywhere on the body.
Inverse psoriasis causes smooth patches of red, inflamed skin. It appears in the armpits and groin area, under the breasts and around the genitals. This type of psoriasis is more common in overweight people.
Pustular psoriasis causes white blisters or pustules surrounded by red skin. This type can be localized (small areas of the body) or generalized (large areas of the body).
Erythrodermic psoriasis can cover most of your body with a red, peeling rash that can itch or burn intensely. This form occurs in people who have unstable plaque psoriasis and is considered a medical emergency because it can lead to severe illness.
Guttate psoriasis has drop-shaped lesions that are pink in color with a scale on top. The lesions appear suddenly, usually following an illness such as strep throat or upper respiratory infection.
What are Psoriasis symptoms and signs?
Psoriasis symptoms and signs include scaly skin plaques, itching, and pain. Read about types, treatment, causes, diet tips, diagnosis, and prognosis. Psoriasis is an autoimmune condition that affects the skin. It occurs when the immune system mistakes healthy skin cells for pathogens and sends out faulty signals that cause overproduction of new skin cells.
Psoriasis can be a chronic disease with periods of remissions and flares. There are different types of psoriasis. Each type has different symptoms. Common psoriasis symptoms include red patches of skin covered with thick silvery scales, dry cracked skin that may bleed, itching and soreness, thickened or ridged nails and stiff joints. The most common type of psoriasis is called plaque psoriasis and it makes up about 90% of cases.
Symptoms typically develop slowly and appear as one or more small red bumps that grow bigger and thicker, eventually becoming inflamed lesions covered in silvery scales. Psoriatic lesions most commonly develop on the knees, elbows, lower back, torso and scalp but can also appear on any area including the fingernails or toenails, palms or soles of the feet or genitals.
What does Psoriasis look like?
 These skin patches are typically red, itchy, and scaly. On people with darker skin the patches may be purple in colour. Psoriasis varies in severity from small, localized patches to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as Koebner phenomenon.
These skin patches are typically red, itchy, and scaly. On people with darker skin the patches may be purple in colour. Psoriasis varies in severity from small, localized patches to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as Koebner phenomenon.
Nails are affected in most people with psoriasis at some point in time. This may include pits in the nails or changes in nail color. Psoriasis can also cause inflammation of the joints, which is known as psoriatic arthritis.
Can Psoriasis affect my joints?
Psoriasis is a chronic skin condition that can also affect the nails and joints. In fact, up to 30% of people with psoriasis may have joint inflammation that produces symptoms of arthritis. The joint symptoms of psoriasis are called psoriatic arthritis.
Although psoriatic arthritis may affect any joint, it occurs most often in the joints at the ends of the fingers and toes. You may also develop a painful, sausage-shaped swelling of your fingers and toes known as dactylitis.
Psoriatic arthritis can range from relatively mild to very severe, depending on how much joint damage has occurred. The most common form of psoriatic arthritis causes pain, stiffness and swelling in your fingers and toes.
Can Psoriasis affect only my nails?
Yes, psoriasis can affect your nails. Psoriasis is a common skin condition that causes skin cells to grow too quickly, resulting in thick, white, silvery or red patches of skin. In addition to causing skin problems, psoriasis may also affect the nails. When this happens, it’s called nail psoriasis or psoriatic nail disease. Nail psoriasis affects about half of all people who have psoriasis that appears on their skin and about 80% of people who have a related joint condition called psoriatic arthritis.
Nail psoriasis often appears as horizontal pits (small depressions) in your fingernails or toenails. This is due to a loss of cells in the nail matrix that produce the nail plate (the hard part of the nail). In severe cases, your nail may become discolored and crumble as it detaches from the nail bed. Your doctor will diagnose nail psoriasis after a physical exam and possibly a lab test if they suspect you also have psoriatic arthritis.
How do health care professionals diagnose Psoriasis?
Health care professionals often diagnose psoriasis by looking at the skin, scalp, and nails. In some cases, health care professionals may recommend a skin biopsy to rule out other disorders and help confirm the diagnosis. To perform the biopsy, a health care professional removes a small piece of skin that is examined under a microscope. Skin biopsies are usually performed in an office or clinic. Smaller patches of psoriasis often develop before larger ones. It often develops on one part of the body first, such as the scalp or knees, and then spreads to other areas. The most common areas affected by plaque psoriasis include:
- Scalp
- Elbows
- Knees
- Lower back
- Soles of feet
- Palms of hands
Eczema vs. Psoriasis
Eczema and psoriasis are not contagious diseases but both involve genetic factors, with an increased incidence in families with allergies or asthma. They also have similar symptoms: patches of irritated skin, itching and redness. However they do not require the same treatment; in fact treating eczema with the drugs used to treat psoriasis can lead to severe complications.
Eczema and psoriasis both cause red, itchy rashes that can be uncomfortable and sometimes painful. But they do have some differences as well as some similarities:
- They’re both linked to allergies and asthma.
- They’re both autoimmune conditions.
- They’re both more common in women than men.
- There are similar treatments for both conditions including topical creams (corticosteroids like hydrocortisone), oral medications (immunosuppressants like methotrex)
Is Psoriasis contagious?
Psoriasis is not contagious. It cannot be passed from person to person. Psoriasis is an immune-mediated condition in which the skin cells grow rapidly, resulting in thick and scaly patches of skin.
Psoriasis is a long-lasting (chronic) disease that can range from mild to severe. The severity of psoriasis varies greatly from person to person. Some people have only a few small patches, while others have large areas of involvement. When people with psoriasis do develop infection, it tends to be more severe than in people without psoriasis.
How many people have Psoriasis?
In the US, there are an estimated 7.5 million people with psoriasis, which equals 2.2% of the population. The incidence is equal in males and females and most prevalent in adults ages 20-49 years old. About one-third of people with psoriasis also have a family member with the disease.
The exact cause is unknown, but it is believed that several factors may be involved: a combination of genetic and environmental factors. Psoriasis occurs when skin cells quickly rise from their origin below the surface of the skin and pile up on the surface before they have a chance to mature.
Psoriasis affects all races; however, it occurs more frequently in whites than in African Americans or Asians. Psoriatic arthritis occurs equally among men and women of all races. Psoriasis is rarely seen in children younger than 10 years old, although infants can be affected by a version of the disorder called napkin psoriasis or diaper psoriasis, characterized by red lesions on the diaper area at age 3 to 4 weeks.
Is there a cure for Psoriasis?
About 30 percent of people who develop psoriasis get it before age 20; however, 50 percent develop the disease between ages 30 and 50. Psoriasis can be very mild or severe enough to affect daily activities such as walking or dressing.
There is no cure for psoriasis, but it can be managed long term with medication or other treatments. People with psoriasis should see a dermatologist for diagnosis and management; this may include discussing treatment options and scheduling regular skin exams to monitor health.
Is Psoriasis hereditary?
According to the National Psoriasis Foundation, psoriasis is an autoimmune disease. This means your immune system attacks healthy cells by mistake. In the case of psoriasis, the T-cells attack the skin cells, causing them to multiply too quickly.
The exact cause of this reaction isn’t known. However, researchers have identified genes that are linked to psoriasis. If you have any of these genes, it doesn’t necessarily mean you’ll develop psoriasis; they’re simply more common in people with the condition.
Inherited traits are passed from parents to children through their genes. In the case of psoriasis, you’re more likely to develop psoriasis if a parent or close relative has had it. The risk increases if both parents have psoriasis.
What healthcare specialists treat Psoriasis?
There’s no cure for psoriasis yet. However, several types of healthcare specialists can help you manage your symptoms and improve the quality of your life. These specialists include dermatologists, rheumatologists and primary care providers (PCPs).
Dermatologists treat diseases of the skin and some cosmetic problems. These doctors diagnose and manage patients with psoriasis. Dermatologists also help patients with psoriasis avoid triggers that make it worse. They often work with rheumatologists to treat more severe forms of psoriasis.
Rheumatologists treat arthritis and other diseases of the joints, muscles and bones. Arthritis means joint inflammation—rheumatic diseases cause aches and pains throughout your body. Rheumatologists focus on how inflammation affects your body as a whole.
What are Psoriasis treatment options?
Treatment options for psoriasis include topical creams and ointments, phototherapy, immunosuppressant drugs, and biologics.
Topical treatments are usually the first line of treatment suggested by a doctor. They include steroid creams or ointments that reduce inflammation and suppression of the immune system at the site of the lesion. These medications may be used in combination with moisturizers to increase their effectiveness.
Phototherapy uses ultraviolet light treatment to slow down cell turnover and reduce inflammation. In this type of therapy, patients are exposed to controlled amounts of UVB and/or UVA light either in a medical office or at home using a UVB lamp or other device.
Immunosuppressants are drugs that suppress the immune system. They can be taken orally or by injection, but they are typically only prescribed when other treatments have failed to work due to the risk of serious side effects.
Biologics are relatively new medications which block specific steps in the immune process that lead to inflammation. They may be administered by injection or intravenously (IV).
What creams, lotions, and home remedies are available for Psoriasis?
There are many products available for psoriasis. However, only some of them are recommended and approved by doctors.
Home remedies include daily bathing in warm water with salts or mineral oil and the application of moisturizers.
Over-the-counter (OTC) products include products containing coal tar, salicylic acid, or anthralin. OTC products are usually not as strong as prescription products. OTC shampoos containing coal tar can help reduce scalp scaling, and a lotion containing colloidal oatmeal can help reduce itching in areas that have small patches of psoriasis.
Prescription medications include corticosteroids (steroids), vitamin D analogues, anthralin, tazarotene, retinoids, calcineurin inhibitors (tacrolimus), and methotrexate. These medications can be prescribed alone or combined with other treatments to increase their effectiveness.
Biologics are new medications that fight inflammation associated with psoriasis and psoriatic arthritis. They target specific parts of the immune system involved in causing joint pain and skin changes. Biologics require an injection or intravenous infusion administered by a health care professional.
Are Psoriasis shampoos available?
Types of psoriasis shampoo
There are several different types of prescription and over-the-counter psoriasis shampoos that can help treat scalp psoriasis. Some of these include:
- salicylic acid shampoos
- coal tar shampoos
- coconut oil based shampoos
- emu oil based shampoos
What oral medications are available for Psoriasis?
Oral medications are available for psoriasis, but they are prescribed less often than topical agents. This is due in large part to the potential side effects of systemic therapies. It is important to weigh the benefits against the risks when considering oral medications. The most common oral treatment for psoriasis is methotrexate (Rheumatrex, Trexall, Otrexup). Other oral medications include cyclosporine (Gengraf, Neoral, Sandimmune) and acitretin (Soriatane).
Is there an anti-psoriasis diet?
Although there is still no cure for psoriasis, there are many things you can do to treat and manage psoriasis. At the top of the list: anti-psoriasis diet.
Some people find that certain foods make their psoriasis better or worse. You may notice that your skin flares up after eating sugary foods or bread, for example. Or maybe dairy products cause your flare-ups.
If you’re not sure which food is causing your psoriasis flare-ups, we’ve come up with several tips on how to figure out which foods you should avoid and which ones you should add to your diet to help manage your symptoms.
Yes and no. A few foods seem to alleviate psoriasis at least temporarily in some people. But these foods do not work for all sufferers, and they do not cure the disease.
The most common foods that help are oily fish, such as salmon and mackerel, according to the National Psoriasis Foundation (NPF). Some other beneficial foods include:
- fruits rich in antioxidants, such as blueberries and cherries
- whole grains
- lean meats, such as turkey and chicken
Foods linked to worsening symptoms include:
- refined carbohydrates, such as white bread and pasta
- red meat
- dairy products
- food additives, including preservatives and artificial sweeteners
What injections or infusions are available for Psoriasis?
Injections and infusions are medications that go straight into your bloodstream. They can be helpful for people who haven’t been able to control their psoriasis with other treatments.
Injecting or infusing medication directly into the bloodstream bypasses the digestive system, so it’s a fast way to get a lot of medicine flowing through your body.
Injections and infusions can be given in your doctor’s office, at an outpatient clinic, or even at home. Some of them have severe side effects, but most people only have minor reactions that are easily treated.
What about light therapy for Psoriasis?
Light therapy has become a mainstay of treatment for psoriasis, with many patients achieving excellent results. In fact, many dermatologists consider it the best treatment available. But there is more to light therapy than meets the eye. The ultraviolet radiation in sunlight and artificial light actually causes skin damage, which is why sunburns are so common. Ultraviolet light also causes premature skin aging and contributes to the risk of skin cancer.
The goal of light therapy for psoriasis is to deliver enough ultraviolet radiation to suppress an overactive immune system without causing significant damage to the skin itself. The ultraviolet radiation used in light therapy is divided into UVA (320-400 nanometers) and UVB (290-320 nanometers). Both types of radiation can cause substantial skin damage, but UVB penetrates much less deeply into the skin than does UVA. This means that UVB does not help as much with widespread psoriasis, because it does not reach all areas of the body.
What are complications of Psoriasis?
Complications from psoriasis include:
Psoriatic arthritis. As many as 30% of people with psoriasis also develop a form of arthritis called psoriatic arthritis. Psoriatic arthritis can cause joint pain and swelling throughout the body but especially in the fingers and toes. It can also cause swelling of tendons (tendonitis) and small joints in the hands and feet. Psoriatic arthritis may be mild or severe enough to affect daily activities and work.
Eye problems. Dry eyes; conjunctivitis (pink eye)
Type 2 diabetes. People with psoriasis appear to have an increased risk of developing type 2 diabetes.
Cardiovascular disease. People who have severe psoriasis — particularly those with psoriatic arthritis — may be more likely to have clogged arteries and other cardiovascular problems than people without the condition.
Obesity. Psoriasis occurs more often in overweight people and those with large waistlines. Obesity can also worsen symptoms of psoriasis.
Metabolic syndrome. This collection of symptoms — which includes high blood pressure, insulin resistance and excess weight around your waist — increases your risk of cardiovascular disease, diabetes and stroke. People with psoriasis have a higher risk of metabolic syndrome than do people without the condition.
Depression and anxiety. These emotional disorders are more common in people who have severe cases of psoriasis compared with those who have milder forms of the disease or no psoriasis at all.
Is it possible to prevent Psoriasis?
There are no known ways to prevent psoriasis. Most people are diagnosed with psoriasis between the ages of 15 and 35, but it can develop at any age. Some people have just a few patches, while others have more severe cases.
Many people notice that their symptoms get worse during cold and dry weather or when they are under stress. Flare-ups may also be triggered by infection, injury to the skin, or medications such as lithium or certain blood pressure drugs.
Psoriasis Clinical Trials
The good news is that there are many clinical trials for psoriasis, and many of them are actively recruiting participants. The bad news is that it’s not easy to figure out which study would be the best match for you.
The psoriasis clinical trials in this section are for individuals who want to help find a cure for psoriasis. All research studies are conducted according to guidelines set forth by the FDA, and are reviewed by an Institutional Review Board (IRB) or a Board of Ethics.
If you have been diagnosed with psoriasis or have a family member who has psoriasis, your participation in one of these clinical trials could further the research being conducted by doctors and scientists at institutions around the world.